Paralytic attacks of Hypokalemic Periodic Paralysis can cause cardiac and/or respiratory distress or arrest. Patients may become unable to cough and may choke on their own secretions or on vomit. Attacks of profound paralysis or ones in which there is cardiac or respiratory distress require immediate emergency medical attention.
First Actions:
- Respiratory and cardiac arrest are possible.
- Check vitals – cardiac diliatation may cause hypotension and low pulse pressure
- Call for Cardiac Monitoring/EKG
- Draw electrolytes to determine serum K+
- Provide 02 – thimble may not reflect 02 saturation due to cardiac dilitation
Monitoring
Measure serum K+ immediately and put electro-cardiographic monitoring in place. The serum K+ level is not always an indication of the severity of the patient’s condition. Some patients experience severe weakness and/or cardiac instability with only mild hypokalemia. Respiratory function may deteriorate rapidly and without warning. The patient must not be left unattended. When the patient is paralyzed swallowing may be compromised and the gag reflex lost. Place the paralyzed patient in the coma position due to the possibility of aspiration. Most deaths in HypoKPP come from aspiration.
Laboratory Studies
Resting membrane potential of muscle fiber in HypoKPP patients is always depolarized from 5-15 mV compared to the normal value of -85 mV. When the serum K+ is lowered it depolarizes muscle fibers further and renders them inexcitable. 1, 2 During an attack, there is usually, but not always, a measurable fall in serum K+, but in some patients the K+ level may never fall below normal. Johnsen’s series of provocative studies recorded an episode of weakness of 11 hours duration provoked by a 0.3 mmol/l fall in the serum K+, and an episode of total paralysis of 19 hours duration provoked by a drop of 1.0 mmol/l. Base your decisions on your patient’s strength and cardiac signs, not on serum potassium levels alone. 1,2,3,4
Treatment
If the patient presents with total paralysis of the extremities but is still able to swallow and breathe adequately, oral sips of KCl solution can be given, 15 to 30 mmol (in children 10 to 15 mmol) in 30 to 60 minute intervals. The release from KCl tablets is too slow. If no improvement is apparent after four to five oral doses, or if nausea or diarrhea occurs after the oral KCl intake, IV administration of KCl is necessary. This also is preferable in patients with acute attacks of paralysis, cardiac distress or ischemia, arrhythmias, difficulties in swallowing and impaired respiration.Using a peripheral vein, the preferred dose for intravenous K+ is 15 mEq (15 mmol) over 15 minutes then 10 mEq/hr (10 mmol/hr) in 500 ml of dilutant. Five percent Mannitol is the solution of choice for IV administration of K+. Mannitol (which is inert) should be used as the solvent (rather than saline or dextrose/glucose, which are both potential triggers of attacks). Infusion must be continued until serum K+ is normal and the patient’s strength returns. Cardiac function must be continuously monitored during IV administration of potassium. 4,5,6,9.
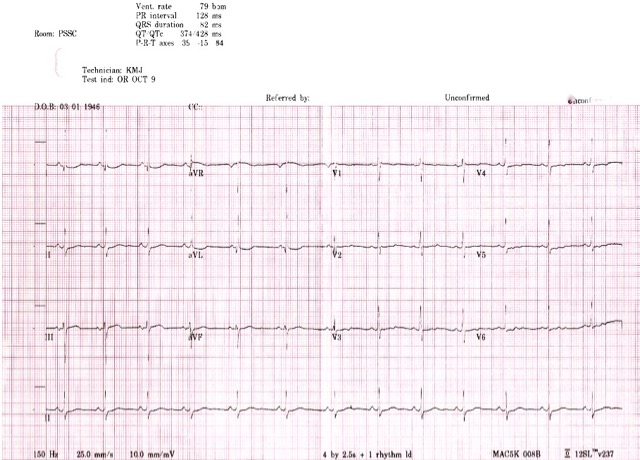
Sinus bradycardia and electrocardiographic (ECG) signs of hypokalemia (U waves in leads II, V-2, V-3, and V-4, progressive flattening of T waves and depression of ST segment) may appear when the serum potassium falls below normal. Prolongation of the PR and QT intervals and T-wave flattening are associated with prominent U-waves.
Johnsen’s study of 106 Danish patients with HypoKPP revealed two patients who developed transient diastolic murmurs during paralysis and another who developed a transient, partial a-v block. He also describes patients who developed bradycardia and unspecified arrhythmias during episodes. 2,4,5,7
In patients with HypoKPP cardiac function can be affected far more seriously during attacks than would be expected from the serum potassium level. The EKG below was done in the ER during an attack of weakness which had not responded to numerous doses of oral potassium over the course of the preceding 12 hours. The patient was a 62-year-old female patient with a history of Hypokalemic Periodic Paralysis. When her serum potassium level came back from the lab it was 4.4 mmol/l, yet the Triage nurse had been unable to get a blood pressure or pulse reading and called Code on the patient. The EKG was done within one minute of arrival in the ER bay. For comparison: EKGs of patients with K+ of 1.7 and 1.8. These are patients without HypoKPP.
Patients should be monitored for several hours after strength is restored, as attacks may reinstate if inadequately treated.
References:
1. Gamstorp, I: Disorders Characterised by Spontaneous Attacks of Weakness Connected with Changes of Serum Potassium; Genetics of Neuromuscular Disorders, pp 175-195 1989; Alan R. Liss Inc.
2. Brooke, M: Introduction to Neuroscience; Lecture Notes AAN 1999
3. Ptacek L.J., et al.: Periodic paralysis. In: Fauci AS, et al, eds. Harrison’s Principles of Internal Medicine. 14th Ed. NYC, McGraw Hill, 1998
4. Schlichtmann, J, Graber, M. University of Iowa Family Practice Handbook, 3rd Edition, Chapter 5, 1999 Hematologic, Electrolyte, and Metabolic Disorders: Potassium.
5. Swash, Michael; Schwartz, Martin S: Neuromuscular Diseases: A practical approach to diagnosis and management; 2nd ed. London; Springer-Verlagg 1988 The Periodic Paralyses pp 344-348
6. Links, Th. P et al; Familial Hypokalemic Periodic Paralysis; Cip-Cegevens Kononklijke Bibliotheek, Den Haag 1992 ISBN 90-9005053-1
7. Johnsen, Torsten; Familial Periodic Paralysis with Hypokalaemia, Danish Medical Bulletin, March 1981 Vol. 28 No. 1
8. Ornato J; Gonzalez ER; Starke H; et al; Incidence and causes of hypokalemia associated with cardiac resuscitation. Am J of Emergency Medicine, Vol 3, Issue 6, Nov 1985, Pages 503-506
9. Griggs RC, Resnick J, Engel WK: Intravenous treatment of hypokalemic periodic paralysis. Arch Neurol 1983, 40(9):539-40.
reviewed and updated 2 May 2022
