*Emergency Treatment of Thyrotoxic Hypokalemic Periodic Paralysis
First Actions:
- Respiratory and cardiac arrest are possible.
- Call for Cardiac Monitoring/EKG
- Draw electrolytes to determine serum K+
- Thyroid studies
- Provide 02 as thimble may not reflect 02 saturation due to cardiac dilitation
A True Endocrine Emergency
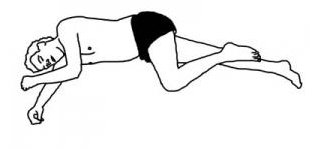
Patients with Thyrotoxic Hypokalemic Periodic Paralysis typically present at the ER with an acute episode of paralysis involving the muscles of the extremities and limb girdles. The lower limbs are more frequently and severely involved than the upper. Weakness may be asymmetrical. Proximal strength is more severely impaired than distal strength.
Cardiac Signs
Consistent with Hypokalemia or Thyrotoxicosis; during paralysis, sinus tachycardia, diffuse ST-T changes, flattening of T waves, prolonged QT intervals, and U waves. Sinus arrest and second-degree atrioventricular block also have been described in patients with THKPP, ventricular fibrillation and ventricular tachycardia.
Thyroid Studies
Elevated total thyroxine, triiodothyronine resin uptake, and total triiodothyronine levels. Radioiodine scan for Graves disease and adenomas.
Treatment
The mainstay of emergency treatment has always been potassium replacement, however not all patients respond to potassium alone and evidence suggests that combining potassium and propranolol is a more effective therapy, with KCl 10 mEq/h iv in half-saline or Ringer’s and/or KCl 2 g every 2 h, orally, monitoring serum K+ level, to avoid rebound hyperkalemia plus Propranolol 3–4 mg/kg, orally.
Because THKPP patients may develop rebound hyperkalemia K+ replacement therapy should be cautious and should not exceed 90 mEq of KCl per 24 hours unless there is a reason for K+ loss, such as diarrhea, vomiting or diuretic use.
In the Manoukian study (19 patients) all patients remained attack free as long as they took methimazole and propranolol hydrochloride or after radioiodine 131 treatment. Eighteen patients were eventually treated with radioiodine 131 therapy. None of the patients had paralytic episodes after a euthyroid state was achieved.
Nonselective beta-blockers such as propranolol may be useful to prevent attacks of paralysis once patients begin taking antithyroid medications but are not yet euthyroid.
For further information see:
The Man Who Couldn’t Walk: A case study of Thyrotoxic PP by Emergency Physicians
Hypokalemic Periodic Paralysis: Managing Hypokalemic Paralysis
References:
- Bergeron L, Sternbach GL. Thyrotoxic periodic paralysis. Ann Emerg Med. 1988;17:843-845.
- Manoukian, M.A. et al; Clinical and Metabolic Features of Thyrotoxic Periodic Paralysis in 24 Episodes. Archives of Internal Medicine Vol. 159 No. 6, March 22, 1999
- Tassone H, Moulin A, Henderson SO 2004 The pitfalls of potassium replacement in thyrotoxic periodic paralysis: a case report and review of the literature. J Emerg Med 26:157–161
- Birkhahn RH, Gaeta TJ, Melniker L 2000 Thyrotoxic periodic paralysis and intravenous propranolol in the emergency setting. J Emerg Med 18:199–202
- Lu KC, Hsu YJ, Chiu JS, Hsu YD, Lin SH 2004 Effects of potassium supplementation on the recovery of thyrotoxic periodic paralysis. Am J Emerg Med 22:54454–54457
- Shayne P, Hart A 1994 Thyrotoxic periodic paralysis terminated with intravenous propranolol. Ann Emerg Med 24:736–740 PMID: https://pubmed.ncbi.nlm.nih.gov/8092604/
